Prevalence and Risk Factors of Obstructive Sleep Apnea among Patients Attending Tertiary Care Teaching Hospital in Odisha, India: A Retrospective Observational Study
DOI:
https://doi.org/10.54133/ajms.v5i1S.252الكلمات المفتاحية:
Berlin questionnaire، Level 1 sleep study، Obstructive sleep apnea، Urban and rural populationالملخص
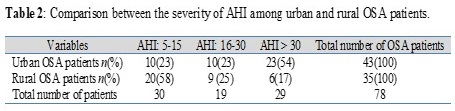
Background: Although obstructive sleep apnea is the most common sleep-disordered breathing, there are fewer studies estimating the prevalence of OSA and its risk factors in urban and rural populations in Odisha. Objective: To estimate the prevalence and risk factors of obstructive sleep apnea in a tertiary care teaching hospital in Odisha, India. Method: It is an observational, retrospective study that was conducted in a sleep study lab for a duration of 4 years (January 2016 to December 2019) by the Department of Physiology and Department of Pulmonology of a tertiary care teaching hospital in Odisha. Patients were first screened for high-risk sleep apnea disorder by the Berlin questionnaire, and then they underwent a level 1 sleep study. Results: Total study patients were 1423, of whom 718 and 705 were from urban and rural areas. The mean age of urban and rural patients was 50.81±12.5 years and 51.63±15.3 years, respectively. The prevalence of OSA in urban areas by AHI criteria was 5.9%, and in rural areas it was 4.9%. The mean AHI of urban OSA patients was 37.86±23.46 and that of rural patients was 16.96±13.8. Conclusion: The prevalence of OSA was higher in urban areas than in rural areas. Both BMI and NC were higher for urban patients than for rural patients. The risk factors were mainly diabetes mellitus and hypertension.
التنزيلات
المراجع
Rodenstein D. Sleep apnoea: traffic and occupational accidents—individual risks, socioeconomic and legal implications. Respiration. 2009;78(3):241-248. doi: 10.1159/000222811.
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230-1235. doi: 10.1056/NEJM199304293281704.
Parish JM, Shepard JW. Cardiovascular effects of sleep disorders. Chest. 1990;97(5):1220-1226. doi: 10.1378/chest.97.5.1220.
Ifergane G, Ovanyan A, Toledano R, Goldbart A, Abu-Salame I, Tal A, Stavsky M, et al. Obstructive sleep apnea in acute stroke: A role for systemic inflammation. Stroke. 2016;47(5):1207-1212. doi: 10.1161/STROKEAHA.115.011749.
Soriano JB, Yáñez A, Renom F, de la Peña M, Gómez A, Duro R, et al. Set up and pilot a population cohort for the study of the natural history of COPD and OSA: the PULSAIB study. Prim Care Respir J. 2010;19(2):140-147. doi: 10.4104/pcrj.2010.00010.
Gay P, Weaver T, Loube D, Iber C. Evaluation of positive airway pressure treatment for sleep-related breathing disorders in adults. Sleep. 2006;29(3):381–3401. doi: 10.1093/sleep/29.3.381.
Kushida CA, Morgenthaler TI, Littner MR, Alessi CA, Bailey D, Coleman J, et al. Practice parameters for the indications for polysomnography and related procedures: An update for 2005. Sleep. 2005;28:499-521. doi: 10.1093/sleep/28.4.499.
Heinzer R, Vat S, Marques‑Vidal P, Marti‑Soler H, Andries D, Tobback N, et al. Prevalence of sleep‑disordered breathing in the general population: The HypnoLaus study. Lancet Resp Med. 2015;3:310‑318. doi: 10.1016/S2213-2600(15)00043-0.
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM, et al. Increased prevalence of sleep‑disordered breathing in adults. Am J Epidemiol. 2013;177:1006‑1014. doi: 10.1093/aje/kws342.
Mirrakhimov AE, Sooronbaev T, Mirrakhimov EM. Prevalence of obstructive sleep apnoea in Asian adults: A systematic review of the literature. BMC Pulm Med. 2013;13:10. doi: 10.1186/1471-2466-13-10.
Udwadia ZF, Doshi AV, Lonkar SG, Singh CI. Prevalence of sleep‑disordered breathing and sleep apnoea in middle‑aged urban Indian men. Am J Respir Crit Care Med. 2004;169:168‑173. doi: 10.1164/rccm.200302-265OC.
Sharma SK, Kumpawat S, Banga A, Goel A. Prevalence and risk factors of obstructive sleep apnoea syndrome in a population of Delhi, India. Chest. 2006;130:149‑156. doi: 10.1378/chest.130.1.149.
Gupta R, Gupta VP. Meta‑analysis of coronary heart disease prevalence in India. Indian Heart J. 1996;48:241‑245. PMID: 8755007.
Mishra S, Joseph RA, Gupta PC, Pezzack B, Ram F, Sinha DN, et al. Trends in bidi and cigarette smoking in India from 1998 to 2015, by age, gender and education. BMJ Glob Health. 2016;1:e000005. doi: 10.1136/bmjgh-2015-000005.
Iber C, Ancoli- Isreal S, Chesson A, Quan S, (Eds.), The AASM Manual for the scoring of sleep and Associated Events, (1st Ed.), Westchester, II; American Academy of Sleep Medicine; 2007.
Nickerson J, Lee E, Nedelman M, Aurora RN, Krieger A, Horowitz CR. Feasibility of portable sleep monitors to detect obstructive sleep apnea (OSA) in a vulnerable urban population HHS public access. J Am Board Fam Med. 2015;28(2):257-264. doi: 10.3122/jabfm.2015.02.140273.
Singh A, Prasad R, Garg R, Kant S, Hosmane GB, Dubey A, et al. A study to estimate prevalence and risk factors of obstructive sleep apnoea syndrome in a semi-urban Indian population. Monaldi Arch Chest Dis. 2017;87:40-48. doi: 10.4081/monaldi.2017.773.
Adesanya AO, Lee W, Greilich NB, Joshi GP. Perioperative management of obstructive sleep apnoea. Chest. 2010;138(6):1489-1498. doi: 10.1378/ chest.10-1108.
Coman AC, Borzan C, Vesa CS, Todea DA. Obstructive sleep apnoea syndrome and the quality of life. Clujul Med. 2016;89(3):390-395. doi: 10.15386/cjmed-593.
Vakulin A, Baulk SD, Catcheside PG, Antic NA, van den Heuvel CJ, et al. Driving simulator performance remains impaired in patients with severe OSA after CPAP treatment. J Clin Sleep Med. 2011;7(3):246-253. doi: 10.5664/ JCSM.1062.
Reddy EV, Kadhiravan T, Mishra HK, Sreenivas V, Handa KK, Sinha S, et al. Prevalence and risk factors of obstructive sleep apnea among middle-aged urban Indians: a community-based study. Sleep Med. 2009;10(8):913-918. doi: 10.1016/j.sleep.2008.08.011.
Sharma SK, Reddy EV, Sharma A, Kadhiravan T, Mishra HK, Sreenivas V, et al. Prevalence and risk factors of syndrome Z in urban Indians. Sleep Med. 2010;11(6):562–568. doi: 10.1016/j.sleep.2010.02.008.
Burgess KR, Havryk A, Newton S, Tsai WH, Whitelaw WA. Targeted case finding for OSA within the primary care setting. J Clin Sleep Med. 2013;9(7):681-686. doi: 10.5664/jcsm.2838.
Devaraj U, Krishnaswamy U, Ramachandran P, Balla S, Pinto A, Venkatnarayan K, et al. Prevalence and risk factors for OSA among urban and rural subjects in Bengaluru District, South India: A Cross-sectional study. Indian J Sleep Med. 2021;16:5-9. doi: 10.5005/jp-journals-10069-0064.
de Paula LK, Alvim RO, Pedrosa RP, Horimoto AR, Krieger JE, Oliveira CM, et al. Heritability of OSA in a rural population. Chest. 2016;149(1):92-97. doi: 10.1378/chest.15- 0843.
Gjevre JA, Pahwa P, Karunanayake C, Hagel L, Rennie D, Lawson J, et al. Excessive daytime sleepiness among rural residents in Saskatchewan. Can Respir J. 2014;21(4):227-233. doi: 10.1155/2014/921541.
Liu J, Wei C, Huang L, Wang W, Liang D, Lei Z, et al. Prevalence of signs and symptoms suggestive of obstructive sleep apnea syndrome in Guangxi, China. Sleep Breath. 2014;18(2):375-382. doi: 10.1007/s11325-013- 0896-2.
Choudhury A, Routray D, Swain S, Das AK. Prevalence and risk factors of people at-risk of obstructive sleep apnea in a rural community of Odisha, India: a community-based cross-sectional study. Sleep Med. 2019;58:42-47. doi: 10.1016/j.sleep.2019.03.014.
Pinto AM, Devaraj U, Ramachandran P, Joseph B, D'Souza GA. Obstructive sleep apnea in a rural population in South India: feasibility of health care workers to administer level III sleep study. Lung India. 2018;35(4):301-306. doi: 10.4103/lungindia.lungindia_433_17.
Rout RN, Bhuyan SK, Priyadarshini A, Bhindhani D, Singh M, Mohapatra S. Obstructive sleep apnea: Dental perspective from upright to supine. J Indian Acad Oral Med Radiol. 2021;33:177-182. doi: 10.4103/jiaomr.jiaomr_254_20.
التنزيلات
منشور
كيفية الاقتباس
إصدار
القسم
الرخصة
الحقوق الفكرية (c) 2023 Al-Rafidain Journal of Medical Sciences

هذا العمل مرخص بموجب Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Published by Al-Rafidain University College. This is an open access journal issued under the CC BY-NC-SA 4.0 license (https://creativecommons.org/licenses/by-nc-sa/4.0/).